The Human View

Integrated Well-Being
The buzz for “wellness” continues to increase in the media, in government, in business, and in insurance. Less noticed, though perhaps more noteworthy, a cadre of intellectuals, scientists, visionaries and post-allopathic physicians are reshaping the dialog of what constitutes well-being. According to these, there are not just financial, but also moral and evolutionary imperatives to re-map the territory defining both individual and societal well-being.
The Institute for Noetic Sciences, founded over 30 years ago by astronaut Edgar Mitchell, will release an important book this fall, Consciousness and Healing: Integral Approaches to Mind-Body Medicine. In the introduction, noted integral thinker Ken Wilber observes:
“The crucial ingredient in any integral medical practice is not the integral medical bag itself – with all the conventional pills, and the orthodox surgery, and the subtle energy medicine, and the acupuncture needles – but the holder of the bag. Body and mind and spirit are operating in self, culture, and nature, and thus health and healing, sickness and wholeness, are all bound up in a multidimensional tapestry that cannot be cut into without loss.”
Are we there yet?
In the June-August issue of Shift: At the Frontiers of Consciousness, Marilyn Schlitz writes: “While science has contributed to our understanding and treatment of disease, it has also served to limit the development of a model in which personal relationships, emotions, meaning, and belief systems are viewed as fundamental points of connection between body, mind, spirit, society, and the environment. For increasing numbers of healthcare consumers and professionals alike, the biomedical model fails to offer a system for understanding the fullness of lived experience – minimizing or negating completely the possibility for human transcendence in the face of illness and disease.”The Institute of HeartMath continues to blaze trails into the largely unmapped territory of the physiology and self-management of human emotions. In a recent “HeartQuotes” e-mail, John Foster Dulles is quoted: “The measure of success is not whether you have a tough problem to deal with, but whether it’s the same problem you had last year.”
Down here on the ground
The re-envisioning of human health and well-being in more integral – or integrated – terms, is underway. Even the stolid insurance industry is beginning to recognize the value and the necessity of expanding its view of what it really means to “manage” care.For many of us, “managed care” has been the like parent whose normal response to their child’s request was, “No! Now, what did you want?” Such an approach has fostered neither trust nor respect. Even as employers begin cautiously to applaud recent reports that average health plan rate increases for 2005 will dip below 10% for the first time since the late 90's – employees are grumbling yet more loudly that this “accomplishment” has come at their direct expense. The leaky dike hasn’t yet been fixed; we’re just using more fingers to plug the holes.
Trigger happy
In the trenches, the emerging trend is towards “population health management.” We want to optimize the utilization of medical resources, the clinical outcome of treatments, and to minimize the costs therefor, all the while promoting and engaging employees in getting healthier and happier – as a group.In a representative population, the cohorts and claims were categorized as follows: "Healthy" people (about 77% of the group) had 5 or fewer ambulatory encounters in a year, and accounted for about 11% of total claims costs. "Episodic" care, which has a defined beginning and endpoint as a "one-time" encounter, plus acute or catastrophic episodes, was needed by 9% of the group, and totalled 38% of claims costs. Members with "chronic needs" (disease state care such as diabetes, coronary artery disease, congestive heart failure, etc.) were only 14% of the group, but 51% of the claims costs! Alarmingly, by 2010, analysts predict that 1 in 4 participants will have chronic needs.
The “management” of these sub-groups is based on diagnosis, treatment, or pharmacological “triggers.” When proposed treatments require pre-certification, when someone enters the hospital for a major illness or acute event, or when certain medications are prescribed, the possibility or expectation of large expenditures “triggers” a pro-active response from the health plan to evaluate the situation and manage the process to maximize both cost efficiency and clinical effectiveness.
Integrated medical management
More meaningful views of health plan activity can emerge when claims processing data, case management data, and disease management data are integrated and analyzed as a whole system. Population risks and claims costs can be stratified, and clinical interventions can be better managed as we recognize, for example, that only X% of our known diabetics are following the clinically-recommended treatment protocols.Integrated medical management is compelling: in a study of 9 health plans' Utilization Review, Care/Case Management, and Disease Management programs, the claims cost savings ranged from 6.4% to 14.5% of total claims - big bucks!
The next logical aspect of this broadened view is to integrate the whole group's health risk factors – both medical and lifestyle – into “business intelligence” engines and predictive modelling tools. Importantly, new “triggers” can now be considered for people who are (for instance) taking high blood pressure or cholesterol-lowering medicines.
The last word
As society’s thought leaders craft a more lofty vision of human well-being, the operational reality at the business and personal levels is also being elevated. Data-supported wellness programs are the next piece of the puzzle. After all, if we want to see the whole picture, all the pieces have to come out of the box.
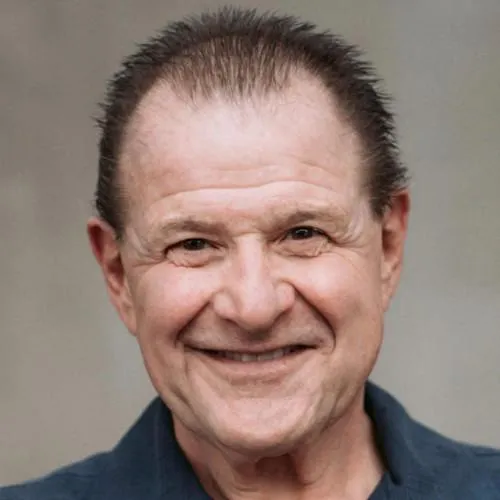
Mark Head
President
With 4 decades of combined experience in employee benefits consulting, wellness and health management, Head brings a unique combination of dynamic perspectives into a clear vision of where the future of health care is moving - and it's moving towards deeper human connection, awareness, and engagement...
Follow Us On
© 2015 - Present, MDH Consulting. All Rights Reserved.
